| Re: Clinical Pharmacology Discussion Thread by Ajoboss(m): 3:46pm On Aug 11, 2019 |
Obinoscopy:
PEDIATRIC PHARMACOLOGY
Children takes drugs thus we need to take special consideration of how the drug works in their body. The way drug works in kids is different from the way it works in an adult. This is because as the organs and systems within the child develops (ontogeny), the pharmacokinetics and pharmacodynamics of drugs changes.
When a child is born until he gets to 1 month he/she is called a neonate. Then from 1 month to 24 months (2 years) he/she is called an infant. From 2 years till 12 years he is called a child. Adolescents are those from 12 years till 18 years. I personally don't see Adolescents as Children but I see them as young adults. Thus my focus will be mostly on those less than 12 years (neonates, infants and children).
Like I said earlier, the organs and systems of a child undergoes different developmental changes from birth till maturity. This changes affect drug disposition when consumed by the child. The most dramatic changes occur in the first 18 months of life. Organs such as the liver and the kidney which play a very critical role in drug metabolism are not fully functional at birth. Also the activities of enzymes such as CYP450 and UGT isoforms is not at maximum. Thus we need to be careful when administering drugs affected by the liver or kidney or the enzymes (CYP & UGT) such as erthromycin, saquinavir, ritonavir, codeine, carbamazepine, etc. to children. A typical example of a pharmacokinetic consideration due to altered renal drug clearance in newborns and infants is in the adminstration of gentamicin. Gentamicin is given every 18-24 hours in neonates and every 6 hours in young children. This is as opposed to how its given to adolescents and young adults (given 8 hourly).
Another factor that contributes to the different drug disposition in kids is the poorly developed Blood Brain Barrier (BBB). Some drugs are crosses the BBB very easily while others don't. Thus this must be taken into consideration when treating a child.
It is also worthy of note that the volume of distribution (Vd) is increased in Infants of 6 months or less. This needs to be taken into account when administering drugs to kids.
The GIT of children is different from those of an adult. For example, gastric pH changes during ontogeny (stomach pH is higher than the adult value due to the immaturity of parietal cells). This is the reason why peroral bioavailability of acid-labile drugs such as penicillin, ampicillin is increased and peroral bioavailability of weak organic acids such as phenobarbital, phenytoin is reduced in kids. Also gastric emptying time is prolonged throughout infancy and childhood due to reduced motility. This delayed emptying time can affect the absorption of drugs with limited water solubility (phenytoin, carbamezepine). Neonates and young infants have problem absorbing fat-soluble vitamins because they don't have adequate bile acids.
ADVERSE DRUG REACTION IN CHILDREN
Drugs can cause adverse reactions when taken by adults and children. This is especially so in children as they don't fully have the body mechanism to deal with these drugs the way adult does. A child is susceptible to ADR indirectly in the womb or during lactation (due to maternal drug exposure) or directly when given a medication.
An example of ADR from maternal drug exposure is the neonatal abstinence syndrome due opioids. Example of ADRs that occur in children are Reyes Syndrome (caused by Aspirin), Serum Sickness (caused by cefaclor), cutaneous toxicity (caused by lamotrigine), hepatotoxicity (caused by valproic acid or paracetamol), cartilage and tendon toxicity (caused by fluoroquinolones).
DRUG USE DURING LACTATION
As I said earlier, a child can indirectly be exposed to a drug during lactation. Fortunately, the concentration of drug achieved in the breast is usually low for most drugs. For these drugs, it is advised that the mother continues breast feeding the child as the benefit of breast feeding outweights the risk. This is because it is known that formula feeding is associated with higher infant morbidity and mortality. For example, in developing countries, HIV mothers who are taking anti-retrovirals should still breast feed their children. This is because the risk of exposing the child to the HIV virus and to the HIV drugs is low compared to the risk of the child dying from not being breast fed.
However there are some drugs that are not to be taken during lactation because they are present in large toxic concentration in the breast milk. These drugs are amiodarone (can affect the child's thyroid function), chloral hydrate (cause drowsiness in the child), chloramphenicol (bone marrow suppression), heroin/methadone (neonatal narcotic dependence), radio active iodine (thyroid suppression), tetracycline (teeth staining), atenolol, niroprusside, clonidine, guanfacine (hypotension), etc.
The following drugs have minimal effect during lactation and thus can be taken by the nurisng mother. They include: penicillins, isoniazid (must be taken with pyridoxine supplement), acyclovir, aspirin, paracetamol, ibuprofen, antacids, albendazole, caffeine, warfarin, oral contraceptives, propranolol, metoprolol, labetalol, enalapril, captopril, methyldopa, nifedipine, amlodipine, cholorothiazide, spironolactone, hydralazine, digoxin chlorpromazine, etc. It is advisable to take the drugs 30 - 60 minutes after breast feeding and 3 - 4 hours before the next feeding.
It is worthy of note that even the drugs that present in large toxic concentration in breast milk can be taken by the lactating mother if prescribed by the doctor. This is especially if the drug is taken for a very short period of time and the mother and baby are properly monitored. Also the drug clonidine has been used off-label as a single post partum dose as a neuraxial analgesia.
Antibiotics such as penicillins, cephalosporins, macrolides and metronidazole are mostly safe. Tetracyclins and flouroquinolones are not safe and should be taken only if benefit outweighs risk and if taken for a short period of time under prescription and proper monitoring of the physician.
Antimalarials such as artesunate, artemether, lumefantrine, quinine, chloroquine are safe to be taken by lactating mothers. They can be taken for prophylaxis or treatment. Also the child being breastfed should be given antimalarials if he has the signs/symptoms. However care should be taking when giving these antimalarials to lactating mothers who's breastfeeding children weighs less than 5kg.
POSOLOGY
People make the mistake of viewing children as little adults. They make adjustments to the dose for a child based on his age (Young's Rule) or weight (Clark's Rule). This is wrong as it may lead to under- or over-dosage. A more reliable way of calculating drug dosage for a child is based on his/her surface area. Aside the surface area, it is important to know the differences in the child's metabolic system compared to an adult as this will enable the doctor and/or the pharmacist to determine the accurate dosage for the child.
Reference
Briggs , Freeman RK, Yaffe SJ: Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk, 10th ed. Wolters Kluwer/Lippincott Williams & Wilkins, 2015.
de Wildt SN et al: Ontogeny of midazolam glucuronidation in preterm infants. Eur J Clin Pharmacol 2010;66:165.
Katzung BG, et al. Basic and Clinical pharmacology, 12 edn. McGraw-Hill, 2012.
Kliegman R, et al. Nelson textbook of pediatrics (Edition 20.). Phialdelphia, PA: Elsevier, 2016.
Koren G. Medication Safety during Pregnancy and Breastfeeding; A Clinician’s Guide, 4th ed. McGraw-Hill, 2006.
So guys this is my piece on pediatric pharmacology. I might do a little writeup on diabetes and hypertension in children as an offshoot of this piece. But that will be at a latter date. Please feel free to let me know if I made any mistake in my writeup as I am not perfect and am amenable to learning. Thanks. nice bro Keep the good work up! 2 Likes 1 Share |
| Re: Clinical Pharmacology Discussion Thread by MTAIYEM: 12:49am On Aug 20, 2019 |
Obinoscopy:
PEDIATRIC PHARMACOLOGY
Children takes drugs thus we need to take special consideration of how the drug works in their body. The way drug works in kids is different from the way it works in an adult. This is because as the organs and systems within the child develops (ontogeny), the pharmacokinetics and pharmacodynamics of drugs changes.
When a child is born until he gets to 1 month he/she is called a neonate. Then from 1 month to 24 months (2 years) he/she is called an infant. From 2 years till 12 years he is called a child. Adolescents are those from 12 years till 18 years. I personally don't see Adolescents as Children but I see them as young adults. Thus my focus will be mostly on those less than 12 years (neonates, infants and children).
Like I said earlier, the organs and systems of a child undergoes different developmental changes from birth till maturity. This changes affect drug disposition when consumed by the child. The most dramatic changes occur in the first 18 months of life. Organs such as the liver and the kidney which play a very critical role in drug metabolism are not fully functional at birth. Also the activities of enzymes such as CYP450 and UGT isoforms is not at maximum. Thus we need to be careful when administering drugs affected by the liver or kidney or the enzymes (CYP & UGT) such as erthromycin, saquinavir, ritonavir, codeine, carbamazepine, etc. to children. A typical example of a pharmacokinetic consideration due to altered renal drug clearance in newborns and infants is in the adminstration of gentamicin. Gentamicin is given every 18-24 hours in neonates and every 6 hours in young children. This is as opposed to how its given to adolescents and young adults (given 8 hourly).
Another factor that contributes to the different drug disposition in kids is the poorly developed Blood Brain Barrier (BBB). Some drugs are crosses the BBB very easily while others don't. Thus this must be taken into consideration when treating a child.
It is also worthy of note that the volume of distribution (Vd) is increased in Infants of 6 months or less. This needs to be taken into account when administering drugs to kids.
The GIT of children is different from those of an adult. For example, gastric pH changes during ontogeny (stomach pH is higher than the adult value due to the immaturity of parietal cells). This is the reason why peroral bioavailability of acid-labile drugs such as penicillin, ampicillin is increased and peroral bioavailability of weak organic acids such as phenobarbital, phenytoin is reduced in kids. Also gastric emptying time is prolonged throughout infancy and childhood due to reduced motility. This delayed emptying time can affect the absorption of drugs with limited water solubility (phenytoin, carbamezepine). Neonates and young infants have problem absorbing fat-soluble vitamins because they don't have adequate bile acids.
ADVERSE DRUG REACTION IN CHILDREN
Drugs can cause adverse reactions when taken by adults and children. This is especially so in children as they don't fully have the body mechanism to deal with these drugs the way adult does. A child is susceptible to ADR indirectly in the womb or during lactation (due to maternal drug exposure) or directly when given a medication.
An example of ADR from maternal drug exposure is the neonatal abstinence syndrome due opioids. Example of ADRs that occur in children are Reyes Syndrome (caused by Aspirin), Serum Sickness (caused by cefaclor), cutaneous toxicity (caused by lamotrigine), hepatotoxicity (caused by valproic acid or paracetamol), cartilage and tendon toxicity (caused by fluoroquinolones).
DRUG USE DURING LACTATION
As I said earlier, a child can indirectly be exposed to a drug during lactation. Fortunately, the concentration of drug achieved in the breast is usually low for most drugs. For these drugs, it is advised that the mother continues breast feeding the child as the benefit of breast feeding outweights the risk. This is because it is known that formula feeding is associated with higher infant morbidity and mortality. For example, in developing countries, HIV mothers who are taking anti-retrovirals should still breast feed their children. This is because the risk of exposing the child to the HIV virus and to the HIV drugs is low compared to the risk of the child dying from not being breast fed.
However there are some drugs that are not to be taken during lactation because they are present in large toxic concentration in the breast milk. These drugs are amiodarone (can affect the child's thyroid function), chloral hydrate (cause drowsiness in the child), chloramphenicol (bone marrow suppression), heroin/methadone (neonatal narcotic dependence), radio active iodine (thyroid suppression), tetracycline (teeth staining), atenolol, niroprusside, clonidine, guanfacine (hypotension), etc.
The following drugs have minimal effect during lactation and thus can be taken by the nurisng mother. They include: penicillins, isoniazid (must be taken with pyridoxine supplement), acyclovir, aspirin, paracetamol, ibuprofen, antacids, albendazole, caffeine, warfarin, oral contraceptives, propranolol, metoprolol, labetalol, enalapril, captopril, methyldopa, nifedipine, amlodipine, cholorothiazide, spironolactone, hydralazine, digoxin chlorpromazine, etc. It is advisable to take the drugs 30 - 60 minutes after breast feeding and 3 - 4 hours before the next feeding.
It is worthy of note that even the drugs that present in large toxic concentration in breast milk can be taken by the lactating mother if prescribed by the doctor. This is especially if the drug is taken for a very short period of time and the mother and baby are properly monitored. Also the drug clonidine has been used off-label as a single post partum dose as a neuraxial analgesia.
Antibiotics such as penicillins, cephalosporins, macrolides and metronidazole are mostly safe. Tetracyclins and flouroquinolones are not safe and should be taken only if benefit outweighs risk and if taken for a short period of time under prescription and proper monitoring of the physician.
Antimalarials such as artesunate, artemether, lumefantrine, quinine, chloroquine are safe to be taken by lactating mothers. They can be taken for prophylaxis or treatment. Also the child being breastfed should be given antimalarials if he has the signs/symptoms. However care should be taking when giving these antimalarials to lactating mothers who's breastfeeding children weighs less than 5kg.
POSOLOGY
People make the mistake of viewing children as little adults. They make adjustments to the dose for a child based on his age (Young's Rule) or weight (Clark's Rule). This is wrong as it may lead to under- or over-dosage. A more reliable way of calculating drug dosage for a child is based on his/her surface area. Aside the surface area, it is important to know the differences in the child's metabolic system compared to an adult as this will enable the doctor and/or the pharmacist to determine the accurate dosage for the child.
Reference
Briggs , Freeman RK, Yaffe SJ: Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk, 10th ed. Wolters Kluwer/Lippincott Williams & Wilkins, 2015.
de Wildt SN et al: Ontogeny of midazolam glucuronidation in preterm infants. Eur J Clin Pharmacol 2010;66:165.
Katzung BG, et al. Basic and Clinical pharmacology, 12 edn. McGraw-Hill, 2012.
Kliegman R, et al. Nelson textbook of pediatrics (Edition 20.). Phialdelphia, PA: Elsevier, 2016.
Koren G. Medication Safety during Pregnancy and Breastfeeding; A Clinician’s Guide, 4th ed. McGraw-Hill, 2006.
So guys this is my piece on pediatric pharmacology. I might do a little writeup on diabetes and hypertension in children as an offshoot of this piece. But that will be at a latter date. Please feel free to let me know if I made any mistake in my writeup as I am not perfect and am amenable to learning. Thanks. More energy and wisdom to you bro. Thanks. |
| Re: Clinical Pharmacology Discussion Thread by Nobody: 6:32am On Aug 30, 2019 |
That was when Nairaland was sane. Imbeciles have taken over now. 1 Like |
| Re: Clinical Pharmacology Discussion Thread by Aaronzy: 9:38am On Aug 30, 2019 |
Please, what is the triple therapy regimen for peptic ulcer disease |
| Re: Clinical Pharmacology Discussion Thread by Nobody: 3:42pm On Aug 30, 2019 |
Pharmacologist
Am I welcome here ? |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 11:04pm On Sep 02, 2019 |
Ajoboss:
nice bro
Keep the good work up! MTAIYEM:
More energy and wisdom to you bro.
Thanks. Thanks bro. |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 11:22pm On Sep 02, 2019 |
horpeyemmi66:
Interested,
Physiologist, Dental Surgery Aspirant AUNafada:
I'm a 500level medical Student and interested in this thread... Motunemotun:
Pharmacologist
Am I welcome here ? You are hereby inducted to this honorable thread. We are most honored to have you. Welcome. The medical community look forward to sharing knowledge with you. See updated list: https://www.nairaland.com/5289692/clinical-pharmacology-discussion-thread#80073865CLINICAL PHARMACOLOGY DISCUSSION THREAD MEMBERS
Obinoscopy - Pharmacist/Epidemiologist
Charliejose - Pharmacology Student
Aysuccess99 - Medical Student Aspirant
Brini - Medical Student
Zenti99 - Medical Student Aspirant
Damitism - Pharmacy Student
Teecube - Pharmacy Student
Eloghosa78 - Medical Student Aspirant
Passion007 - Medical Doctor
Samgreguc - Pharmacy Student
Eyideejay - Medical Student
ULQUIORRA - MSc Pharmacology Student
Tolugar - Physiologist/Pharmacologist
Fostermd - Medical Doctor (Psychiatrist/Neuropsychopharmacologist)
Ajpharm - Pharmacy Student
Thefarr - Veterinary Doctor
Captainnigeria - Pharmacy Student Aspirant
Gbosaa - Herbalist
Adaminedens - Medical Doctor
YMCgyna - Pharmacy Student
DrClay - Medical Doctor
Breezy90 - Pharmacy Student
Edyza - Anatomist/MSc Clinical Pharmacology Student
Lebienconnu - Medical Student
Kunlexic - Pharmacy Student Aspirant
Arsenate - Pharmacist/MSc Pharmacology Student Aspirant
Razzydoo - MSc Pharmacology (in view)
Usen9c - Chemist
Sakaguchi - Medical Student
Itzpretzy - Pharmacy Student
Hustla242 - Clinical Pharmacologist
Dungdusugyang - Medical Biochemist
GogetterMD - Medical Doctor
Quatermaine - Medical Student
Cnwamo - Nurse/Medical Student
Imperiouxx - Biochemist
Hensben - Pharmacologist
Frankyskyboi - Pharmacist
Ochek - Nurse
DonJ2 - Medical Lab Scientist
Aieromon - Pharmacist
JoannaSedley - Nurse/Anaesthetician/Doctor of Nursing (In View)
Swashi007 - Pharmacy Student
Debuscket - Radiographer
Johnsonpac - Biochemist
Tekel - Human Anatomist
JellyBean190 - Medical Doctor
Nnewi1stSon - Pharmacist
DebhariJones - Interim Pharmacist
ADUBA1 - Health and Environment
Babymillenium - Nurse
Philtrum - Medical Student
Liverpoolfc - Human physiologist
Xkid2000 - Pharmacist student
Drfash - Medical Student
Tebill - Biochemist/Medical doctor
Deltaboy10 - Medical Student
Tydd - Interim Pharmacist
Godwinigweh - Nursing Student
Yahbas83 - Medical Student
Waloma - Nurse
Mbatagr82 - Medical lab Science Student
Xoctic - Medical Student
Winzor78 - Medical Student
Igwedexy - Physiology
Lexo22 - Biochemist
Leward - Medical Student
FutureDon - Neuroscientist
Shollyps - Biochemistry Student
Firstolalekan - MSc Clinical Pharmacology Aspirant
Rxfemi - Pharmacist
Godfreykingsley - Anatomist
Greenslicks - Counselling Psychologist
Adeoladrg - Pharmacy Student
Kennymighty - Clinical Biochemist
Anselm791 - Medical Student
Johncuppa - Chemist/Pharmacy Student Aspirant
Mzdharmey - Pharmacology Student
Kinxlink - Pharmacology Aspirant
Mesther96 - Pharmacology Student
Winbyforce - Physician/Pharmacologist
Crispinkc - Dental Student
Armani03 - Medical biochemist Student
Man100 - Microbiologist
Tygood - Physiology Student
Bioduneberry - Chemist
CircleOfWilis - Medical doctor
Ekpekus - Medical doctor/Msc. Pharmacology
AGgal - Nurse/Midwife
Baebyfaze91 - Pharmacist student
Linguist - Nurse (accident& emergency)
Tfun - Nursing Student
DrAmanda - Medical Student
Somtea - Pharmacist
Abdulsalax - Pharmacist Aspirant
ProfEinstein - Physiotherapist
Mashad - Anatomist
Amaham - Anaesthesiologist
Kenshin17 - Biochemistry
Kristana - Pharmacist Student
1k001 - General Physician
Biolaolowo - Medical Student
Delpharm - Pharmacist Student
Desy24444 - Nurse
Tycoon4 - Intern. Pharmacist
Dynasty92 - Pharmacist Student
Tushqueen - Radiographer
Cmanforall - Clinical Pharmacologist Aspirant
Sisiafrika - Pharmacy Student
Akkylod - Medical Student
Tieeeboy - Human Anatomy Student
Tosodus - Medical Lab Tech/Biochemist/Medical Student Aspirant
Boluzie - Medical Student
Guldberg - Dental Surgery Student
Dadinho - MSc Pharmacology Aspirant
Shazily012 - Physiologist
Cxp - Medical Student
shollish - Pharmacy Student
Blessgod30 - Pharmacist
Jerryvyne - Pharmacy Student
Vicmed1 - Medical Student
Thewhizzkid1 - Medical Student
MTAIYEM - Clinical Student
Exynos - Medical Aspirant
Horpeyemmi66 - Physiologist/Dental Surgery Aspirant
AUNafada - Medical Student
Motunemotun - Pharmacologist
1 Like |
| Re: Clinical Pharmacology Discussion Thread by Nobody: 2:16pm On Sep 11, 2019 |
please can the outter virgina(around her public hair) of a lady contain hiv virus. |
| Re: Clinical Pharmacology Discussion Thread by Nobody: 8:17pm On Sep 11, 2019 |
spendoon:
please can the outter virgina(around her public hair) of a lady contain hiv virus. use condoms, abstain and stop asking foolish questions 1 Like |
| Re: Clinical Pharmacology Discussion Thread by Nobody: 9:17pm On Sep 11, 2019 |
spendoon:
please can the outter virgina(around her public hair) of a lady contain hiv virus.    |
| Re: Clinical Pharmacology Discussion Thread by BoluwajiPieters: 1:27am On Sep 20, 2019 |
Obinoscopy:
This is because beta blockers are known to reduce insulin secretion at the pancreas and decrease insulin sensitivity. The beta-2 adrenergic receptors is known to play a role in insulin release thus any beta blocker that has some affinity for beta-2 receptor can worsen diabetic treatment.
Its interesting to note that alpha adrenergic receptors does the opposite.
Reference:
Das, V.A., Robinson, R. & Paulose, C.S. Enhanced β-adrenergic receptors in the brain and pancreas during pancreatic regeneration in weanling rats. Mol Cell Biochem (2006) 289: 11. https://doi.org/10.1007/s11010-006-9142-6 Plus Beta blockers mask the symptoms of hypoglycemia in that, for a known diabetic patient on OHAs/insulin therapy and concurrently using beta blockers, when hypoglycemia occurs, the alarming symptoms the patient is supposed to experience such as tachycardia, tremor and all will not be experienced by the patient as a result of beta blockade. This puts the patient at a higher risk of hypoglycemic coma. 2 Likes |
| Re: Clinical Pharmacology Discussion Thread by BoluwajiPieters: 1:32am On Sep 20, 2019 |
Aaronzy:
Please, what is the triple therapy regimen for peptic ulcer disease
Triple therapy is a cocktail of three drugs used in the management of PUD. It includes a proton pump inhibitor (PPI) such as lansoprazole, Omeprazole and rabeprazole which inhibits the final step in gastric acid secretion hence reducing gastric acid secretion and increasing gastric PH. It also includes the use of antibiotics in the eradication of Helicobacter pylori which is an etiological bacteria in PUD. Amoxicillin, Clarithromycin, metronidazole, tinidazole are some of the antibiotics used in combination with the PPI. |
|
| Re: Clinical Pharmacology Discussion Thread by Nobody: 4:40pm On Jan 29, 2020 |
Well-done. Nice to find myself here. Please I want to ask the brand/market name of drug with Sulphadoxine Pyrimethamine for prevention of malaria that one can find in Nigeria. Also, if anyone knows very potent herbs, one or two, that cure/prevent malaria that malaria parasites are not resistant to in Nigeria.
Thanks |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 3:50pm On Oct 10, 2020 |
Obinoscopy:
You are hereby inducted to this honorable thread. We are most honored to have you. Welcome. The medical community look forward to sharing knowledge with you.
See updated list: https://www.nairaland.com/5289692/clinical-pharmacology-discussion-thread#80073865
Wow, it's been a while I last updated this thread. I think this thread need to be resuscitated. I will try and post something on the Clinical Pharmacology of Renal Disease in a weeks time. I also enjoin everyone to be active. You can also post something on any topic of your choice. We are all here to learn and share knowledge. 3 Likes |
| Re: Clinical Pharmacology Discussion Thread by LucaB: 4:43pm On Oct 10, 2020 |
Obinoscopy:
Wow, it's been a while I last updated this thread. I think this thread need to be resuscitated. I will try and post something on the Clinical Pharmacology of Renal Disease in a weeks time. I also enjoin everyone to be active. You can also post something on any topic of your choice. We are all here to learn and share knowledge. |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 9:08pm On Oct 18, 2020 |
Obinoscopy:
Wow, it's been a while I last updated this thread. I think this thread need to be resuscitated. I will try and post something on the Clinical Pharmacology of Renal Disease in a weeks time. I also enjoin everyone to be active. You can also post something on any topic of your choice. We are all here to learn and share knowledge. Like I promised, I'll now go ahead and post my notes on Clinical Pharmacology of Renal Disease. 1 Like |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 9:11pm On Oct 18, 2020 |
CLINICAL PHARMACOLOGY OF RENAL DISEASE
The kidney is a very important organ in our body despite its small size. It helps with the removal of waste products and maintains homoestasis. The kidney filter the extracelluar fluid volume across the renal glomeruli an average of 12 times a day. The kidney has a very important role in blood pressure regulation (via the renin-angiotensin-aldosterone system RAAS), in red blood cell production (via the production of erythropoietin) and in bone formation/remodelling (via the hydroxylation of vitamin D to its active form: 1, 25 dihydro Vitamin D). This means that anyone with kidney issues might have lots of problems such as hypertension, osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency, etc). Also, some of the drugs we take need to be metabolised and/or excreted by the kidney, thus those drugs either need to be stopped or their dosing frequency or strength reduced else they could be toxic. As pharmacologists, we need to know these drugs. I will list some of them here.
There are two type of renal disease, the acute renal disease and the chronic renal disease. From the name, the difference between the two is the onset duration. For acute, it takes hours to days to develop while for chronic it takes months to years to develop. I will dwell more on the chronic form (generally called Chronic Kidney Disease or CKD for short) as it’s the most common and the most insidious.
Like I said earlier, CKD is a progressive loss of kidney function over a period of months or years. Approximately 30 million US adults (more than one in seven) have CKD – the risk is highest in African-Americans and other non-Caucasians. As usual, we don’t have any reliable data for Nigeria – which is sad as lots and lots of people have kidney issues in this country. An evidence to this fact is the number of celebrities that have kidney issues (OJB Jezreel, Muna Obiekwe, Biglo, Fred Ekata, Samuel Adesanya, Emma Ugolee, Leo Mezie, Prince James Uche, Gbenga Ajumoko). However, it is estimated that about 10% of the world’s population is affected by CKD. End Stage Renal Disease (ESRD) is the most advanced stage of CKD. At this stage, the only solution is either dialysis or kidney transplant else the patient will die.
The most common cause of CKD is diabetes. This is followed closely by hypertension. Also some drugs can cause kidney disease. These drugs are: Aminoglycosides, Amphotericin B, Cisplatin, Cyclosporine, Loop Diuretics, NSAIDs, Polymyxins, Radiographic Contrast Dyes, Tacrolimus, Vancomycin, etc. Of all these drugs, I’d say NSAIDs are the heavy culprit because of its accessibility and rampant use and misuse.
The functional unit of the kidney is the nephron. Each nephron comprises the glomerulus, the proximal and distal convoluted tubule, the descending and ascending loop of henle, and the collecting duct. Filtration occurs at the glomerulus while reabsorption occurs at the loop of henle and convoluted tubules. Substances with molecular weight < 40000 daltons (including most drugs) can pass through the glomerular capillaries, larger substances (protein and protein bound drugs) are filtered out. The protein albumin is ideally supposed to be filtered out at the glomerulus due to its large size. If the glomerulus is damaged however, some albumin passes into the urine (albuminuria). The amount of albumin in the urine is used along with the Glomerular Filtration Rate (GFR) to assess the severity of kidney disease. We also use Blood Urea Nitrogen (BUN) and Serum Creatinine (SCr) to assess severity of kidney disease. The Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend using GFR, degree of albuminuria and cause of CKD to determine the degree/stage of renal impairments (there are 5 stages). A GFR < 60ml/min/1.73m2 and/or albuminuria (albumin excretion rate AER ≥ 30) indicates that the patient has CKD and specific treatment is warranted to prevent progression of the disease.
Angiotensin Converting Enzyme Inhibitors (ACEIs) or Angiotensin Receptor Blockers (ARBs) are firstline drugs to prevent progression of disease in patients with CKD, diabetes or hypertension if albuminuria is present. Patients with stage 5 has kidney failure (ESRD) which requires either dialysis or transplant only.
During treatment, there is need to also address the possible complications of CKD such as osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency). Treatment mostly requires supplementation with the deficient substance (vitamin D – Calcitriol, Cinacalcet, erythropoietin – Epoetin Alfa, Darbepoetin Alfa, etc) and/or the use of binders to remove excesses (Phosphate Binders such as Aluminium Hydroxide, Calcium Acetate, Calcium Carbonate, Ferric Citrate, etc., Potassium Removers such as Furosemide, Sodium Polystyrene Sulfonate, Patiromer, Dialysis, etc.). Treatment of hyperkalemia actually involves 3 steps. Step one is the stabilizing the heart with Calcium Gluconate, step two is moving some of the potassium into the cells using Insulin + Dextrose, Sodium Bicarbonate and Albuterol, and step three is removing the remaining excess potassium out of the body using Diuretics or Potassium Removers. Metabolic acidosis is treated using Sodium Bicarbonate and Sodium Citrate/Citric Acid solution.
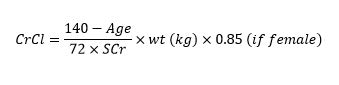
Certain drugs are contraindicated in CKD. This is primarily because those drugs are metabolised by the kidney thus they will accumulate in patients with CKD and elicit immense toxic effect. What we mostly use to determine if a drug is contraindicated or not is Creatinine Clearance (CrCl) which is calculated using the Cockcroft-Gault Equation. The equation is stated below:
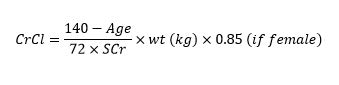
Drugs like NItrofurantoin is contraindicated if CrCl < 60 ml/min, Voriconazole IV is contraindicated if CrCl < 50 ml/min, Tenofovir Disproxil Fumarate is contraindicated if < 50 ml/min, Tenofovir Alafenamide is contraindicated if < 30 ml/min. Other medications contraindicated when CrCl < 30 ml/min include NSAIDs, Dabigatran (when used for treatment of deep vein thrombosis and pulmonary embolism, DVT/PE), Rivaroxaban (when used for treatment of DVT/PE), Bisphosphonates, Duloxetine, Potassium Sparing Diuretics, Tramadol, etc. Note that Tenofovir has two different forms, the Disoproxil Fumarate form is affected more by CKD than the Alafenamide form. So we should be aware of the HIV brands that has either form. Brands that has the Disoproxil Fumarate form are Viread, Truvada, Atripla, Complera, Stribild while brands that has the Alafenamide form include Descovy, Bictarvy, Genvoya, etc.
Besides CrCl, we also use the estimated Glomerular Filtration Rate (eGFR) to estimate kidney function when dosing certain medications. The equation for eGFR is provided below:

Drugs like Metformin, Sodium Glucose coTransporter 2 inhibitors (SGLT2i) , Meperidine, etc. are contraindicated if eGFR < 30ml/min/1.73m2
As can be seen from both formulas for CrCl and eGFR, they can be easily measured. All you need is the serum creatinine level, the rest (age, weight, sex, race) are pretty easy to measure. It is highly recommended that either CrCl or eGFR is measured for patients about to commence these medications.
There are drugs that are not contraindicated in CKD but rather require dosing modifications (ie reduction in dose). I will list some of them here: Fluconazole, Quinolones (except Moxifloxacin), Metoclopramide, Aminoglycosides, Beta-Lactam Antibiotics (except Anti-Staphylococcal Penicillins and Ceftriazone), Enoxaparins (Low Molecular Weight Heparins, LMWHs), Bisphosphonates, Lithium, Famotidine, Ranitidine, Rivaroxaban (when used for treatment of Atrial Fibrillation, AFib), Apixaban (when used for treatment of AFib), Dabigatran (when used for treatment of AFib), etc. For these drugs, we are to reduce the dose to prevent toxicity. Sometimes, the dose reduction can even get up to 40 – 50% or more. For Aminoglycosides, rather than reducing the dose in CKD, its preferable to increase the dosing interval (eg from tid to bid). Thankfully, there are drugs that are not metabolised by the kidney so we don’t have to worry about reducing their dose. It is preferable to give those drugs to patients with CKD. Some of those drugs include: Moxifloxacin, Anti-Staphylococcal Penicillins (Nafcillin, Oxacillin), Ceftriazone, Metoprolol, Carbamazepine, Zolpidem, Fentanyl, Levomethadone, Amiodarone, Pioglitazone, Gliclazide, Gliquidone, etc.
As I said earlier, if CKD progresses to failure (stage 5 disease), dialysis is required in all patients who do not receive a kidney transplant. The two primary type of dialysis are hemodialysis and peritoneal dialysis. In hemodialysis, we use a dialyzer while in peritoneal, we use the patient’s peritoneal membrane as the dialyzer. During peritoneal dialysis, the dialysis solution (usually containing glucose) is pumped into the peritoneal cavity. The solution is left in the abdomen to dwell for a period of time, then is drained. This cycle is repeated throughout the day, every day. When a patient receives dialysis, we must consider the amount of medication cleared during dialysis in order to recommend the correct dose and interval. Medications that are removed during dialysis (including many antibiotics) must be given after dialysis or may require a supplemental dose following dialysis. Drug removal during dialysis depends on the following factors:
1. molecular weight: smaller molecules are more readily removed by dialysis
2. volume of distribution (Vd): drugs with large Vd are less likely to be removed by dialysis
3. protein-binding: highly protein-bound drugs are less likely to be removed by dialysis
In conclusion, CKD is highly prevalent in Nigeria. Its progress is very insidious, thus there is need for us to actively monitor our patients renal function. This involves calculating a patients CrCl and/or eGFR and also ascertaining other comorbidities such as hypertension, diabetes, etc. As drug experts, we need to know drugs that are contraindicated in CKD as well as drugs that can cause or worsen CKD. We also need to know drugs whose metabolism depends on renal function as their dosage will be affected in patients with CKD. CKD treatment is multifactorial, it involves treating all possible comorbidities and signs/symptoms. Stage 5 CKD can also be treated using dialysis or kidney transplant.
REFERENCE
Brunton LL, et al. The Pharmacological Basis of Therapeutics, 13th edn. McGraw-Hill, 2018.
Hartmann B, et al. Drug Therapy in Patients with Chronic Renal Failure. Dtsch Arztebl Intl. 2010;107(37):647-656.
Katzung BG, et al. Basic Clinical Pharmacology, 14th edn. McGraw-Hill, 2018.
KDIGO CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Inter., Suppl. 2013;3:1-150.
Mula-Abed WS, et al. Estimated Glomerular Filtration Rate (GFR): A Serum Creatinine-Based Test for the Detection of Chronic Kidney Disease and its Impact on Clinical Practice. Oman Med J. 2012;27(2):108-113.
Zeind CS, Carvalho MG, et al. Applied Therapeutics: The Clinical Use of Drugs, 11th edn. Wolters Kluwer, 2018. cc: Nairaland medical community . 5 Likes |
| Re: Clinical Pharmacology Discussion Thread by Liverpoolfc(m): 1:28pm On Oct 27, 2020 |
Obinoscopy:
CLINICAL PHARMACOLOGY OF RENAL DISEASE
The kidney is a very important organ in our body despite its small size. It helps with the removal of waste products and maintains homoestasis. The kidney filter the extracelluar fluid volume across the renal glomeruli an average of 12 times a day. The kidney has a very important role in blood pressure regulation (via the renin-angiotensin-aldosterone system RAAS), in red blood cell production (via the production of erythropoietin) and in bone formation/remodelling (via the hydroxylation of vitamin D to its active form: 1, 25 dihydro Vitamin D). This means that anyone with kidney issues might have lots of problems such as hypertension, osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency, etc). Also, some of the drugs we take need to be metabolised and/or excreted by the kidney, thus those drugs either need to be stopped or their dosing frequency or strength reduced else they could be toxic. As pharmacologists, we need to know these drugs. I will list some of them here.
There are two type of renal disease, the acute renal disease and the chronic renal disease. From the name, the difference between the two is the onset duration. For acute, it takes hours to days to develop while for chronic it takes months to years to develop. I will dwell more on the chronic form (generally called Chronic Kidney Disease or CKD for short) as it’s the most common and the most insidious.
Like I said earlier, CKD is a progressive loss of kidney function over a period of months or years. Approximately 30 million US adults (more than one in seven) have CKD – the risk is highest in African-Americans and other non-Caucasians. As usual, we don’t have any reliable data for Nigeria – which is sad as lots and lots of people have kidney issues in this country. An evidence to this fact is the number of celebrities that have kidney issues (OJB Jezreel, Muna Obiekwe, Biglo, Fred Ekata, Samuel Adesanya, Emma Ugolee, Leo Mezie, Prince James Uche, Gbenga Ajumoko). However, it is estimated that about 10% of the world’s population is affected by CKD. End Stage Renal Disease (ESRD) is the most advanced stage of CKD. At this stage, the only solution is either dialysis or kidney transplant else the patient will die.
The most common cause of CKD is diabetes. This is followed closely by hypertension. Also some drugs can cause kidney disease. These drugs are: Aminoglycosides, Amphotericin B, Cisplatin, Cyclosporine, Loop Diuretics, NSAIDs, Polymyxins, Radiographic Contrast Dyes, Tacrolimus, Vancomycin, etc. Of all these drugs, I’d say NSAIDs are the heavy culprit because of its accessibility and rampant use and misuse.
The functional unit of the kidney is the nephron. Each nephron comprises the glomerulus, the proximal and distal convoluted tubule, the descending and ascending loop of henle, and the collecting duct. Filtration occurs at the glomerulus while reabsorption occurs at the loop of henle and convoluted tubules. Substances with molecular weight < 40000 daltons (including most drugs) can pass through the glomerular capillaries, larger substances (protein and protein bound drugs) are filtered out. The protein albumin is ideally supposed to be filtered out at the glomerulus due to its large size. If the glomerulus is damaged however, some albumin passes into the urine (albuminuria). The amount of albumin in the urine is used along with the Glomerular Filtration Rate (GFR) to assess the severity of kidney disease. We also use Blood Urea Nitrogen (BUN) and Serum Creatinine (SCr) to assess severity of kidney disease. The Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend using GFR, degree of albuminuria and cause of CKD to determine the degree/stage of renal impairments (there are 5 stages). A GFR < 60ml/min/1.73m2 and/or albuminuria (albumin excretion rate AER ≥ 30) indicates that the patient has CKD and specific treatment is warranted to prevent progression of the disease.
Angiotensin Converting Enzyme Inhibitors (ACEIs) or Angiotensin Receptor Blockers (ARBs) are firstline drugs to prevent progression of disease in patients with CKD, diabetes or hypertension if albuminuria is present. Patients with stage 5 has kidney failure (ESRD) which requires either dialysis or transplant only.
During treatment, there is need to also address the possible complications of CKD such as osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency). Treatment mostly requires supplementation with the deficient substance (vitamin D – Calcitriol, Cinacalcet, erythropoietin – Epoetin Alfa, Darbepoetin Alfa, etc) and/or the use of binders to remove excesses (Phosphate Binders such as Aluminium Hydroxide, Calcium Acetate, Calcium Carbonate, Ferric Citrate, etc., Potassium Removers such as Furosemide, Sodium Polystyrene Sulfonate, Patiromer, Dialysis, etc.). Treatment of hyperkalemia actually involves 3 steps. Step one is the stabilizing the heart with Calcium Gluconate, step two is moving some of the potassium into the cells using Insulin + Dextrose, Sodium Bicarbonate and Albuterol, and step three is removing the remaining excess potassium out of the body using Diuretics or Potassium Removers. Metabolic acidosis is treated using Sodium Bicarbonate and Sodium Citrate/Citric Acid solution.
Certain drugs are contraindicated in CKD. This is primarily because those drugs are metabolised by the kidney thus they will accumulate in patients with CKD and elicit immense toxic effect. What we mostly use to determine if a drug is contraindicated or not is Creatinine Clearance (CrCl) which is calculated using the Cockcroft-Gault Equation. The equation is stated below:
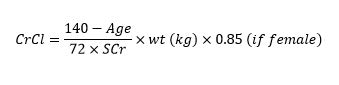
Drugs like NItrofurantoin is contraindicated if CrCl < 60 ml/min, Voriconazole IV is contraindicated if CrCl < 50 ml/min, Tenofovir Disproxil Fumarate is contraindicated if < 50 ml/min, Tenofovir Alafenamide is contraindicated if < 30 ml/min. Other medications contraindicated when CrCl < 30 ml/min include NSAIDs, Dabigatran (when used for treatment of deep vein thrombosis and pulmonary embolism, DVT/PE), Rivaroxaban (when used for treatment of DVT/PE), Bisphosphonates, Duloxetine, Potassium Sparing Diuretics, Tramadol, etc. Note that Tenofovir has two different forms, the Disoproxil Fumarate form is affected more by CKD than the Alafenamide form. So we should be aware of the HIV brands that has either form. Brands that has the Disoproxil Fumarate form are Viread, Truvada, Atripla, Complera, Stribild while brands that has the Alafenamide form include Descovy, Bictarvy, Genvoya, etc.
Besides CrCl, we also use the estimated Glomerular Filtration Rate (eGFR) to estimate kidney function when dosing certain medications. The equation for eGFR is provided below:

Drugs like Metformin, Sodium Glucose coTransporter 2 inhibitors (SGLT2i) , Meperidine, etc. are contraindicated if eGFR < 30ml/min/1.73m2
As can be seen from both formulas for CrCl and eGFR, they can be easily measured. All you need is the serum creatinine level, the rest (age, weight, sex, race) are pretty easy to measure. It is highly recommended that either CrCl or eGFR is measured for patients about to commence these medications.
There are drugs that are not contraindicated in CKD but rather require dosing modifications (ie reduction in dose). I will list some of them here: Fluconazole, Quinolones (except Moxifloxacin), Metoclopramide, Aminoglycosides, Beta-Lactam Antibiotics (except Anti-Staphylococcal Penicillins and Ceftriazone), Enoxaparins (Low Molecular Weight Heparins, LMWHs), Bisphosphonates, Lithium, Famotidine, Ranitidine, Rivaroxaban (when used for treatment of Atrial Fibrillation, AFib), Apixaban (when used for treatment of AFib), Dabigatran (when used for treatment of AFib), etc. For these drugs, we are to reduce the dose to prevent toxicity. Sometimes, the dose reduction can even get up to 40 – 50% or more. For Aminoglycosides, rather than reducing the dose in CKD, its preferable to increase the dosing interval (eg from tid to bid). Thankfully, there are drugs that are not metabolised by the kidney so we don’t have to worry about reducing their dose. It is preferable to give those drugs to patients with CKD. Some of those drugs include: Moxifloxacin, Anti-Staphylococcal Penicillins (Nafcillin, Oxacillin), Ceftriazone, Metoprolol, Carbamazepine, Zolpidem, Fentanyl, Levomethadone, Amiodarone, Pioglitazone, Gliclazide, Gliquidone, etc.
As I said earlier, if CKD progresses to failure (stage 5 disease), dialysis is required in all patients who do not receive a kidney transplant. The two primary type of dialysis are hemodialysis and peritoneal dialysis. In hemodialysis, we use a dialyzer while in peritoneal, we use the patient’s peritoneal membrane as the dialyzer. During peritoneal dialysis, the dialysis solution (usually containing glucose) is pumped into the peritoneal cavity. The solution is left in the abdomen to dwell for a period of time, then is drained. This cycle is repeated throughout the day, every day. When a patient receives dialysis, we must consider the amount of medication cleared during dialysis in order to recommend the correct dose and interval. Medications that are removed during dialysis (including many antibiotics) must be given after dialysis or may require a supplemental dose following dialysis. Drug removal during dialysis depends on the following factors:
1. molecular weight: smaller molecules are more readily removed by dialysis
2. volume of distribution (Vd): drugs with large Vd are less likely to be removed by dialysis
3. protein-binding: highly protein-bound drugs are less likely to be removed by dialysis
In conclusion, CKD is highly prevalent in Nigeria. Its progress is very insidious, thus there is need for us to actively monitor our patients renal function. This involves calculating a patients CrCl and/or eGFR and also ascertaining other comorbidities such as hypertension, diabetes, etc. As drug experts, we need to know drugs that are contraindicated in CKD as well as drugs that can cause or worsen CKD. We also need to know drugs whose metabolism depends on renal function as their dosage will be affected in patients with CKD. CKD treatment is multifactorial, it involves treating all possible comorbidities and signs/symptoms. Stage 5 CKD can also be treated using dialysis or kidney transplant.
REFERENCE
Brunton LL, et al. The Pharmacological Basis of Therapeutics, 13th edn. McGraw-Hill, 2018.
Hartmann B, et al. Drug Therapy in Patients with Chronic Renal Failure. Dtsch Arztebl Intl. 2010;107(37):647-656.
Katzung BG, et al. Basic Clinical Pharmacology, 14th edn. McGraw-Hill, 2018.
KDIGO CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Inter., Suppl. 2013;3:1-150.
Mula-Abed WS, et al. Estimated Glomerular Filtration Rate (GFR): A Serum Creatinine-Based Test for the Detection of Chronic Kidney Disease and its Impact on Clinical Practice. Oman Med J. 2012;27(2):108-113.
Zeind CS, Carvalho MG, et al. Applied Therapeutics: The Clinical Use of Drugs, 11th edn. Wolters Kluwer, 2018.
cc: Nairaland medical community
Good write up. It would have been better if there were citation. It would have been more useful to research students. 2 Likes |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 3:35pm On Oct 27, 2020 |
Liverpoolfc:
Good write up. It would have been better if there were citation. It would have been more useful to research students. That's true. It would require more work though. |
| Re: Clinical Pharmacology Discussion Thread by Jman06(m): 8:53am On Nov 01, 2020 |
Following |
| Re: Clinical Pharmacology Discussion Thread by Uyi168: 10:42am On Nov 01, 2020 |
Well-done. Nice to find myself here. Please I want to ask the brand/market name of drug with Sulphadoxine Pyrimethamine for prevention of malaria that one can find in Nigeria. Also, if anyone knows very potent herbs, one or two, that cure/prevent malaria that malaria parasites are not resistant to in Nigeria.
Thanks .. The different common brands containing sulphadoxine and pyrimentamine include.: Swidar. Amalar. Suresidar. Melofan. Maldox.. Etc. 1 Like |
| Re: Clinical Pharmacology Discussion Thread by Strugglingman: 2:54pm On Nov 01, 2020 |
Obinoscopy:
Wow, it's been a while I last updated this thread. I think this thread need to be resuscitated. I will try and post something on the Clinical Pharmacology of Renal Disease in a weeks time. I also enjoin everyone to be active. You can also post something on any topic of your choice. We are all here to learn and share knowledge. weldone sir Its been a while |
| Re: Clinical Pharmacology Discussion Thread by Strugglingman: 2:58pm On Nov 01, 2020 |
Obinoscopy:
CLINICAL PHARMACOLOGY OF RENAL DISEASE
The kidney is a very important organ in our body despite its small size. It helps with the removal of waste products and maintains homoestasis. The kidney filter the extracelluar fluid volume across the renal glomeruli an average of 12 times a day. The kidney has a very important role in blood pressure regulation (via the renin-angiotensin-aldosterone system RAAS), in red blood cell production (via the production of erythropoietin) and in bone formation/remodelling (via the hydroxylation of vitamin D to its active form: 1, 25 dihydro Vitamin D). This means that anyone with kidney issues might have lots of problems such as hypertension, osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency, etc). Also, some of the drugs we take need to be metabolised and/or excreted by the kidney, thus those drugs either need to be stopped or their dosing frequency or strength reduced else they could be toxic. As pharmacologists, we need to know these drugs. I will list some of them here.
There are two type of renal disease, the acute renal disease and the chronic renal disease. From the name, the difference between the two is the onset duration. For acute, it takes hours to days to develop while for chronic it takes months to years to develop. I will dwell more on the chronic form (generally called Chronic Kidney Disease or CKD for short) as it’s the most common and the most insidious.
Like I said earlier, CKD is a progressive loss of kidney function over a period of months or years. Approximately 30 million US adults (more than one in seven) have CKD – the risk is highest in African-Americans and other non-Caucasians. As usual, we don’t have any reliable data for Nigeria – which is sad as lots and lots of people have kidney issues in this country. An evidence to this fact is the number of celebrities that have kidney issues (OJB Jezreel, Muna Obiekwe, Biglo, Fred Ekata, Samuel Adesanya, Emma Ugolee, Leo Mezie, Prince James Uche, Gbenga Ajumoko). However, it is estimated that about 10% of the world’s population is affected by CKD. End Stage Renal Disease (ESRD) is the most advanced stage of CKD. At this stage, the only solution is either dialysis or kidney transplant else the patient will die.
The most common cause of CKD is diabetes. This is followed closely by hypertension. Also some drugs can cause kidney disease. These drugs are: Aminoglycosides, Amphotericin B, Cisplatin, Cyclosporine, Loop Diuretics, NSAIDs, Polymyxins, Radiographic Contrast Dyes, Tacrolimus, Vancomycin, etc. Of all these drugs, I’d say NSAIDs are the heavy culprit because of its accessibility and rampant use and misuse.
The functional unit of the kidney is the nephron. Each nephron comprises the glomerulus, the proximal and distal convoluted tubule, the descending and ascending loop of henle, and the collecting duct. Filtration occurs at the glomerulus while reabsorption occurs at the loop of henle and convoluted tubules. Substances with molecular weight < 40000 daltons (including most drugs) can pass through the glomerular capillaries, larger substances (protein and protein bound drugs) are filtered out. The protein albumin is ideally supposed to be filtered out at the glomerulus due to its large size. If the glomerulus is damaged however, some albumin passes into the urine (albuminuria). The amount of albumin in the urine is used along with the Glomerular Filtration Rate (GFR) to assess the severity of kidney disease. We also use Blood Urea Nitrogen (BUN) and Serum Creatinine (SCr) to assess severity of kidney disease. The Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend using GFR, degree of albuminuria and cause of CKD to determine the degree/stage of renal impairments (there are 5 stages). A GFR < 60ml/min/1.73m2 and/or albuminuria (albumin excretion rate AER ≥ 30) indicates that the patient has CKD and specific treatment is warranted to prevent progression of the disease.
Angiotensin Converting Enzyme Inhibitors (ACEIs) or Angiotensin Receptor Blockers (ARBs) are firstline drugs to prevent progression of disease in patients with CKD, diabetes or hypertension if albuminuria is present. Patients with stage 5 has kidney failure (ESRD) which requires either dialysis or transplant only.
During treatment, there is need to also address the possible complications of CKD such as osteoporosis, anemia, and diseases due to poor homoestasis (eg hyperphosphatemia, hyperkalemia, metabolic acidosis, vitamin D deficiency). Treatment mostly requires supplementation with the deficient substance (vitamin D – Calcitriol, Cinacalcet, erythropoietin – Epoetin Alfa, Darbepoetin Alfa, etc) and/or the use of binders to remove excesses (Phosphate Binders such as Aluminium Hydroxide, Calcium Acetate, Calcium Carbonate, Ferric Citrate, etc., Potassium Removers such as Furosemide, Sodium Polystyrene Sulfonate, Patiromer, Dialysis, etc.). Treatment of hyperkalemia actually involves 3 steps. Step one is the stabilizing the heart with Calcium Gluconate, step two is moving some of the potassium into the cells using Insulin + Dextrose, Sodium Bicarbonate and Albuterol, and step three is removing the remaining excess potassium out of the body using Diuretics or Potassium Removers. Metabolic acidosis is treated using Sodium Bicarbonate and Sodium Citrate/Citric Acid solution.
Certain drugs are contraindicated in CKD. This is primarily because those drugs are metabolised by the kidney thus they will accumulate in patients with CKD and elicit immense toxic effect. What we mostly use to determine if a drug is contraindicated or not is Creatinine Clearance (CrCl) which is calculated using the Cockcroft-Gault Equation. The equation is stated below:
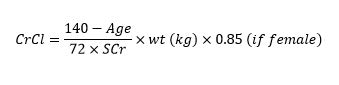
Drugs like NItrofurantoin is contraindicated if CrCl < 60 ml/min, Voriconazole IV is contraindicated if CrCl < 50 ml/min, Tenofovir Disproxil Fumarate is contraindicated if < 50 ml/min, Tenofovir Alafenamide is contraindicated if < 30 ml/min. Other medications contraindicated when CrCl < 30 ml/min include NSAIDs, Dabigatran (when used for treatment of deep vein thrombosis and pulmonary embolism, DVT/PE), Rivaroxaban (when used for treatment of DVT/PE), Bisphosphonates, Duloxetine, Potassium Sparing Diuretics, Tramadol, etc. Note that Tenofovir has two different forms, the Disoproxil Fumarate form is affected more by CKD than the Alafenamide form. So we should be aware of the HIV brands that has either form. Brands that has the Disoproxil Fumarate form are Viread, Truvada, Atripla, Complera, Stribild while brands that has the Alafenamide form include Descovy, Bictarvy, Genvoya, etc.
Besides CrCl, we also use the estimated Glomerular Filtration Rate (eGFR) to estimate kidney function when dosing certain medications. The equation for eGFR is provided below:

Drugs like Metformin, Sodium Glucose coTransporter 2 inhibitors (SGLT2i) , Meperidine, etc. are contraindicated if eGFR < 30ml/min/1.73m2
As can be seen from both formulas for CrCl and eGFR, they can be easily measured. All you need is the serum creatinine level, the rest (age, weight, sex, race) are pretty easy to measure. It is highly recommended that either CrCl or eGFR is measured for patients about to commence these medications.
There are drugs that are not contraindicated in CKD but rather require dosing modifications (ie reduction in dose). I will list some of them here: Fluconazole, Quinolones (except Moxifloxacin), Metoclopramide, Aminoglycosides, Beta-Lactam Antibiotics (except Anti-Staphylococcal Penicillins and Ceftriazone), Enoxaparins (Low Molecular Weight Heparins, LMWHs), Bisphosphonates, Lithium, Famotidine, Ranitidine, Rivaroxaban (when used for treatment of Atrial Fibrillation, AFib), Apixaban (when used for treatment of AFib), Dabigatran (when used for treatment of AFib), etc. For these drugs, we are to reduce the dose to prevent toxicity. Sometimes, the dose reduction can even get up to 40 – 50% or more. For Aminoglycosides, rather than reducing the dose in CKD, its preferable to increase the dosing interval (eg from tid to bid). Thankfully, there are drugs that are not metabolised by the kidney so we don’t have to worry about reducing their dose. It is preferable to give those drugs to patients with CKD. Some of those drugs include: Moxifloxacin, Anti-Staphylococcal Penicillins (Nafcillin, Oxacillin), Ceftriazone, Metoprolol, Carbamazepine, Zolpidem, Fentanyl, Levomethadone, Amiodarone, Pioglitazone, Gliclazide, Gliquidone, etc.
As I said earlier, if CKD progresses to failure (stage 5 disease), dialysis is required in all patients who do not receive a kidney transplant. The two primary type of dialysis are hemodialysis and peritoneal dialysis. In hemodialysis, we use a dialyzer while in peritoneal, we use the patient’s peritoneal membrane as the dialyzer. During peritoneal dialysis, the dialysis solution (usually containing glucose) is pumped into the peritoneal cavity. The solution is left in the abdomen to dwell for a period of time, then is drained. This cycle is repeated throughout the day, every day. When a patient receives dialysis, we must consider the amount of medication cleared during dialysis in order to recommend the correct dose and interval. Medications that are removed during dialysis (including many antibiotics) must be given after dialysis or may require a supplemental dose following dialysis. Drug removal during dialysis depends on the following factors:
1. molecular weight: smaller molecules are more readily removed by dialysis
2. volume of distribution (Vd): drugs with large Vd are less likely to be removed by dialysis
3. protein-binding: highly protein-bound drugs are less likely to be removed by dialysis
In conclusion, CKD is highly prevalent in Nigeria. Its progress is very insidious, thus there is need for us to actively monitor our patients renal function. This involves calculating a patients CrCl and/or eGFR and also ascertaining other comorbidities such as hypertension, diabetes, etc. As drug experts, we need to know drugs that are contraindicated in CKD as well as drugs that can cause or worsen CKD. We also need to know drugs whose metabolism depends on renal function as their dosage will be affected in patients with CKD. CKD treatment is multifactorial, it involves treating all possible comorbidities and signs/symptoms. Stage 5 CKD can also be treated using dialysis or kidney transplant.
REFERENCE
Brunton LL, et al. The Pharmacological Basis of Therapeutics, 13th edn. McGraw-Hill, 2018.
Hartmann B, et al. Drug Therapy in Patients with Chronic Renal Failure. Dtsch Arztebl Intl. 2010;107(37):647-656.
Katzung BG, et al. Basic Clinical Pharmacology, 14th edn. McGraw-Hill, 2018.
KDIGO CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Inter., Suppl. 2013;3:1-150.
Mula-Abed WS, et al. Estimated Glomerular Filtration Rate (GFR): A Serum Creatinine-Based Test for the Detection of Chronic Kidney Disease and its Impact on Clinical Practice. Oman Med J. 2012;27(2):108-113.
Zeind CS, Carvalho MG, et al. Applied Therapeutics: The Clinical Use of Drugs, 11th edn. Wolters Kluwer, 2018.
cc: Nairaland medical community
impressive 1 Like |
| Re: Clinical Pharmacology Discussion Thread by Obinoscopy(m): 6:34am On Dec 27, 2021 |
Hi guys, I'm doing a little reading on cough, cold and catarrh. Perhaps I'll do little writeup on them when I get the chance. 2 Likes |
| Re: Clinical Pharmacology Discussion Thread by Strugglingman: 12:11pm On Dec 29, 2021 |
Obinoscopy:
Hi guys, I'm doing a little reading on cough, cold and catarrh. Perhaps I'll do little writeup on them when I get the chance. okay boss |
| Re: Clinical Pharmacology Discussion Thread by NLegendforte: 5:02am On Feb 05, 2024 |
Wonderful thread. Revive the thread please. |
| Re: Clinical Pharmacology Discussion Thread by Isobug: 7:45am On Feb 05, 2024 |
So we have this type of interesting and educative thread here |
| Re: Clinical Pharmacology Discussion Thread by NLegendforte: 8:25pm On Feb 05, 2024 |
Isobug:
So we have this type of interesting and educative thread here This thread must be revived 1 Like |